Published online Oct 21, 2010. doi: 10.3748/wjg.v16.i39.4992
Revised: July 3, 2010
Accepted: July 10, 2010
Published online: October 21, 2010
AIM: To perform a meta-analysis to answer whether long-term recurrence rates after laparoscopic-assisted surgery are comparable to those reported after open surgery.
METHODS: A comprehensive literature search of the MEDLINE database, EMBASE database, and the Cochrane Central Register of Controlled Trials for the years 1991-2010 was performed. Prospective randomized clinical trials (RCTs) were eligible if they included patients with colon cancer treated by laparoscopic surgery vs open surgery and followed for more than five years.
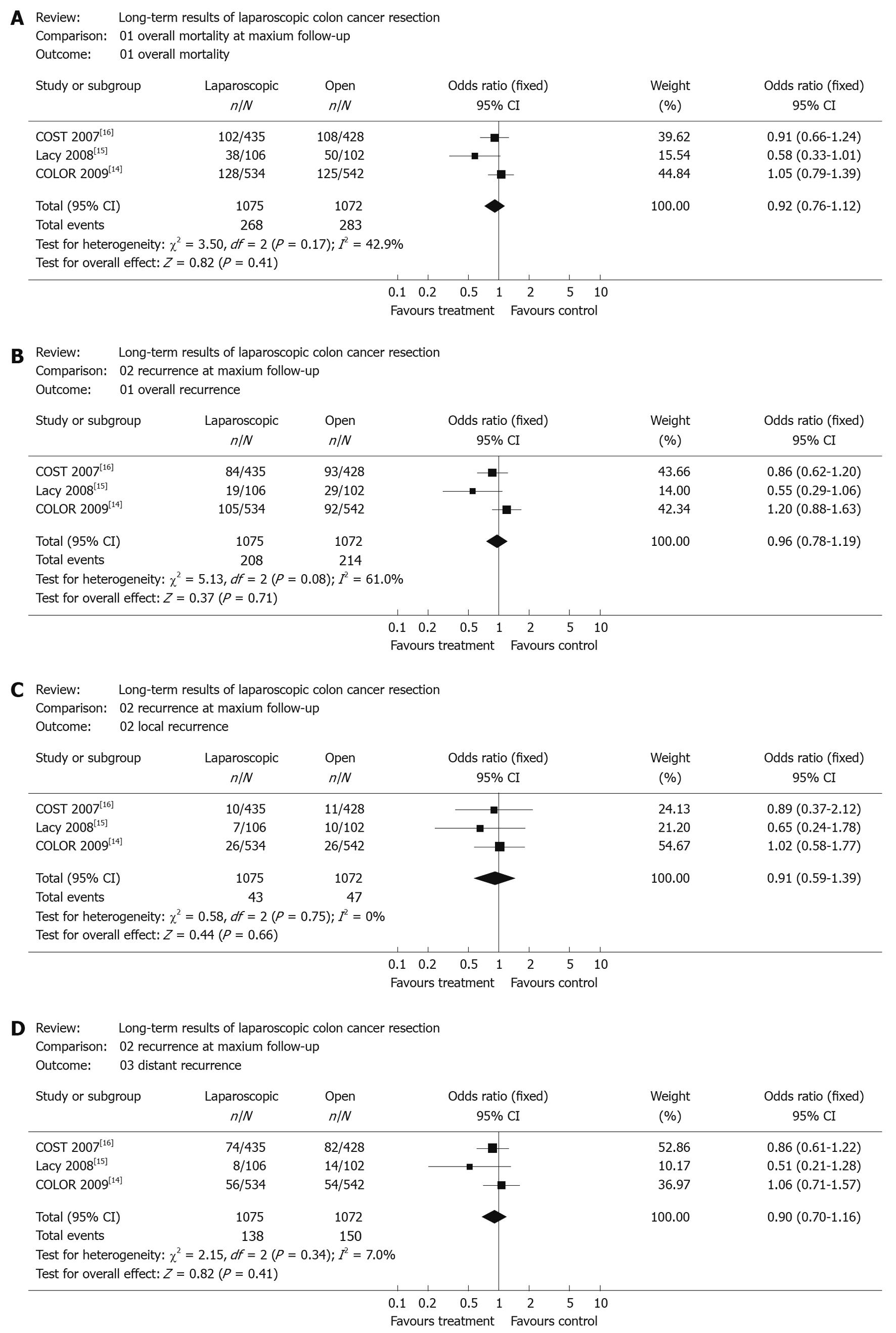
RESULTS: Three studies involving 2147 patients reported long-term outcomes based on five-year data and were included in the analysis. The overall mortality was similar in the two groups (24.9%, 268/1075 in the laparoscopic group and 26.4%, 283/1072 in open group). No significant differences between laparoscopic and open surgery were found in overall mortality during the follow-up period of these studies [OR (fixed) 0.92, 95% confidence intervals (95% CI): 0.76-1.12, P = 0.41]. No significant difference in the development of overall recurrence was found in colon cancer patients, when comparing laparoscopic and open surgery [2147 pts, 19.3% vs 20.0%; OR (fixed) 0.96, 95% CI: 0.78-1.19, P = 0.71].
CONCLUSION: This meta-analysis suggests that laparoscopic surgery was as efficacious and safe as open surgery for colon cancer, based on the five-year data of these included RCTs.
- Citation: Bai HL, Chen B, Zhou Y, Wu XT. Five-year long-term outcomes of laparoscopic surgery for colon cancer. World J Gastroenterol 2010; 16(39): 4992-4997
- URL: https://www.wjgnet.com/1007-9327/full/v16/i39/4992.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i39.4992
Colon cancer is the third most common malignancy in men and women[1]. Traditionally, cancers of the colon were removed through large abdominal incisions. Since the advent of laparoscopic surgery, it has become clear that patients benefit from a minimally invasive approach in a variety of ways[2]. In 1991, laparoscopic-assisted colectomy (LAC) was first reported[3,4]. Short-term advantages of laparoscopic colorectal surgery compared to conventional surgery are well known, and include less pain, better pulmonary function, shorter duration of postoperative ileus, less fatigue and a better quality of life[5-8].
However, it was uncertain whether there would be a long-term survival difference. Several large trials have been reported which discuss the long-term survival difference. The primary aim of these trials is to test the hypothesis that disease-free survival and overall survival are equivalent, regardless of whether patients receive laparoscopic-assisted or open colectomy. The second aim is to assess the recurrence of cancer. The objective of this systematic review is to assess that in the long-term, laparoscopic-assisted colon resection for cancer is not inferior to open colectomy with respect to cancer survival and recurrence. The main outcome of concern is overall mortality and recurrence.
A comprehensive literature search of the MEDLINE database, EMBASE database, and the Cochrane Central Register of Controlled Trials for the years 1991-2010 was performed. Searches were carried out using medical subject headings (MeSH) and free text words in combination with the search strategy for randomised controlled trials (RCT). The following search was adapted for each database: laparoscopy [MeSH], surgery [MeSH], colon [MeSH], colectomy [MeSH], restorative proctocolectomy [MeSH], and colonic neoplasms [MeSH]. Reference lists from the trials were hand-searched to identify further relevant trials. The following selection criteria were applied: (1) study design: RCTs reported with relevant information available; (2) study population: patients with colon cancer; (3) intervention: laparoscopic surgery vs open surgery; (4) samples more than 100 patients; and (5) follow-up more than five years.
Two authors independently evaluated all included trials using a list of selected quality items assessing components of internal validity. Method of randomization, concealment of random allocation, blinding of outcome assessors and reporting of an intention-to-treat analysis were assessed. Trials were considered to be of good quality if they reported on three or four of these quality items, of moderate quality if they reported on one or two items, and of low quality if they reported none of the items. The reporting of this systematic review is in accordance with the QUOROM statement[9].
Treatment effects were expressed as risk ratios with corresponding 95% confidence intervals (95% CI). Where possible, outcomes were pooled with a fixed effects model and random effects model. Heterogeneity was assessed using the χ2 statistic and the proportion of variation due to heterogeneity was expressed as I2. In the absence of significant heterogeneity (P > 0.05 for χ2), fixed-effects model (inverse variance method) was used, and in the presence of significant heterogeneity (P < 0.05 for χ2) and random effects (DerSimonian-Laird method) models. If substantial heterogeneity was found in the included studies, the result was reported from the random effects model. A P value of 0.05 was used as the cut-off value to determine statistical significance. The meta-analyses were performed by using Review Manager 4.2 provided by The Cochrane Collaboration. If data for meta-analysis was considered inappropriate in the included studies, some outcomes were presented in a descriptive way.
Funnel plots were constructed to evaluate potential publication bias using the standard error and diagnostic odds ratio, however, because there are only three studies included, the funnel plots will not be very helpful and will not be shown in the article.
A total of 66 published articles of RCTs comparing laparoscopically assisted and open surgery for colon cancer were identified. Of these trials, there were 19 articles just with short-term outcomes available and another 17 articles with regard to the colorectal cancer. In addition, 21 articles had not reported relevant information. So there were 9 potential articles left to further review. Of these trials, 4 studies were excluded because there were less than 100 patients included[10-13]. Two studies were reported at a different time. So finally 3 studies involving 2147 patients reported long-term outcome data and were included in the analysis. All of the included studies were published as full articles. Baseline characteristics of included studies are described in Table 1. Quality assessment revealed that all studies were of good or moderate quality (Table 2), indicating that all studies were of reasonable methodological quality; none of the studies had any “fatal” methodological flaws.
In 2009, the COLOR trial[14] published its long-term outcomes after laparoscopic surgery vs open surgery. 1076 patients were eligible for analysis (542 assigned open surgery and 534 assigned laparoscopic surgery). Median follow-up was 53 mo (range 0.03-60). The combined 3-year disease-free survival for all stages was 74.2% in the laparoscopic group and 76.2% in the open surgery group (P = 0.70). The hazard ratio (HR) for disease-free survival (open vs laparoscopic surgery) was 0.92 (95% CI: 0.74-1.15). The combined 3-year overall survival for all stages was 81.8% in the laparoscopic group and 84.2% in the open-surgery group (P = 0.45).
In 2008, Lacy et al[15] reported the long-term results of a randomized clinical trial of laparoscopy-assisted vs open surgery (LAC vs OC) for colon cancer. Two hundred and nineteen patients entered the study. The median follow-up was 95 mo. There was a tendency towards higher cancer-related survival (P = 0.07, NS) and overall survival (P = 0.06, NS) for the LAC group. The regression analysis showed that LAC was independently associated with a reduced risk of tumor relapse (hazard ratio 0.47, 95% CI: 0.23-0.94), death from a cancer-related cause (0.44, 0.21-0.92) and death from any cause (0.59, 0.35-0.98). So they concluded that LAC is more effective than OC in the treatment of colon cancer. In 2002, Lacy et al[5] reported the same study with a median length of follow-up of 43 mo, demonstrating that LAC was more effective for treatment of colon cancer in terms of morbidity, hospital stay, tumor recurrence, and cancer-related survival.
In 2007, Fleshman et al[16] published the 5-year data from the COST study group trial. Patients were followed a median of 7 years. Disease-free 5-year survival (OC 68.4%, LAC 69.2%, P = 0.94) and overall 5-year survival (OC 74.6%, LAC 76.4%, P = 0.93) were similar for the 2 groups. Overall recurrence rates were similar for the 2 groups (OC 21.8%, LAC 19.4%, P = 0.25). These recurrences were distributed similarly between the 2 treatment groups. Sites of first recurrence were distributed similarly between the treatment arms (OC: wound 0.5%, liver 5.8%, lung 4.6%, other 8.4%; LAC: wound 0.9%, liver 5.5%, lung 4.6%, other 6.1%). Likewise, in 2004, the three-year outcomes of COST[17] were also reported with the recurrence rate and the overall survival being similar for the two groups. So they concluded that laparoscopic colectomy for curable colon cancer is not inferior to open surgery based on oncologic endpoints.
All 3 studies reported overall mortality at maximum follow-up. 2147 patients were included in this meta-analysis. The overall mortality was similar in the two groups (24.9%, 268/1075 in the laparoscopic group and 26.4%, 283/1072 in the open group). No significant differences between laparoscopic and open surgery were found in overall mortality during the follow-up period of the study [OR (fixed) 0.92, 95% CI: 0.76-1.12, P = 0.41] (Figure 1A). Regarding the cancer-related mortality, only Lacy’s study reported this result (16%, 17/106 in laparoscopic group and 27%, 28/102 in open group, P = 0.07, NS).
Both COLOR and COST trials reported the overall 5-year disease-free survival and overall 5-year survival between laparoscopic and open groups. In the COLOR trial, the overall 5-year disease-free survival and overall 5-year survival were 66.5% vs 67.9% and 73.8% vs 74.2%, respectively; in the COST trial, the overall 5-year disease-free survival and overall 5-year survival were 69.2% vs 68.4% and 76.4% vs 74.6%, respectively. As seen in the two large randomized trials, these two outcomes were similar between the two groups.
All 3 studies reported these outcomes. No significant difference in the development of overall recurrence was found in colon cancer patients, when comparing laparoscopic and open surgery [2147 pts, 19.3% vs 20.0%; OR (fixed) 0.96, 95% CI: 0.78-1.19, P = 0.71] (Figure 1B). The number of patients that developed a local recurrence at the maximum follow-up of the study was similar after laparoscopic and open surgery, showing that there is no significant difference between laparoscopic and open procedures [2147 pts, 4.0% vs 4.4%; OR (fixed) 0.91, 95% CI: 0.59-1.39. P = 0.66] (Figure 1C). Similarly, no significant difference in the development of distant metastases was found in colon cancer patients, when comparing laparoscopic and open surgery [2147 pts, 12.8% vs 14.0%; OR (fixed) 0.90, 95% CI: 0.70-1.16, P = 0.41] (Figure 1D).
Colon cancer is one of the most common cancers in both female and male persons. Treatment involves surgical resection of the segment of the bowel containing the tumor and wide tumor-free margins. Lymph nodes in the area are also removed. Conventional surgery is the mainstream treatment of colorectal cancer and has good survival rates for stage-1 tumors. For many people it is now possible to use video-endoscopic surgery (laparoscopy), which may have short term advantages that include less pain, better pulmonary function, shorter time for return of bowel function (duration of postoperative ileus), less fatigue, and improved convalescence, as suggested in a Cochrane systematic analysis on short-term outcomes[18]. This meta-analysis also demonstrated that postoperative duration of hospital stay is less and quality of life may be improved in the early postoperative course. Furthermore, the risk of postoperative morbidity is decreased by the laparoscopic approach, namely because of a reduced surgical morbidity.
However, the procedure is complex and for colon cancer the long-term results on survival are not known. There are several large RCTs published and several systematic reviews performed to assess the difference between the laparoscopic and open approach. In 2007, Bonjer and his colleague[19] performed a meta-analysis of trials randomizing patients with colon cancer to laparoscopically assisted or open colectomy to determine whether laparoscopic colectomy for cancer is oncologically safe. Patients included in this analysis had at least 3 years of complete follow-up data. Of 1765 patients, 229 were excluded, leaving 796 patients in the laparoscopically assisted arm and 740 patients in the open arm for analysis. Three-year disease-free survival rates in the laparoscopically assisted and open arms were 75.8% and 75.3%, respectively. The 3-year overall survival rate after laparoscopic surgery was 82.2% and after open surgery was 83.5%. Disease-free and overall survival rates for stages I, II, and III evaluated separately did not differ between the 2 treatments. So they concluded that laparoscopically assisted colectomy for cancer is oncologically safe. Again in 2007, Kahnamoui and his colleagues[20] published a systematic review on laparoscopic surgery for colon cancer. The results of this review suggest that, although there is no definitive answer, overwhelming evidence presently indicates that laparoscopic colon cancer resection is as safe and efficacious as the conventional open technique. In 2008, Kuhry and his colleagues[21] published a Cochrane systematic review of randomised controlled trials on the long-term outcomes of laparoscopic surgery for colorectal cancer with the median follow-up from 19-59 mo. No significant difference in tumour recurrence after laparoscopic and open surgery for colon cancer was observed (3 RCTs, hazard ratio for tumour recurrence in the laparoscopic group 0.86; 95% CI: 0.70-1.08). Similarly, in colon cancer patients, no significant differences in overall mortality were found (2 RCTs, hazard ratio for overall mortality after laparoscopic surgery 0.86; 95% CI: 0.86-1.07). So they also concluded that laparoscopic resection of carcinoma of the colon is associated with a long-term outcome that is similar to that after open colectomy.
All 3 systematic reviews demonstrated that laparoscopic colon cancer resection is as safe and efficacious as the conventional open technique in terms of 3-year survival and 3-year disease-free survival and recurrence.
The main objective of this present meta-analysis is to demonstrate that in the long run, laparoscopic colon cancer resection is also as safe and efficacious as open surgery, especially for overall 5-year survival and mortality and recurrence. So the duration of follow-up of all included studies was more than 60 mo, as shown in the table of patient characteristics. There are several characteristics of the three included trials. First, all 3 included trials had a large sample size, especially COST trial (863) and COLOR (1076) trial. Second, the quality of the 3 trials is very high. Third, all of the patients only had colon adenocarcinoma. Additionally, the follow-up was very long. So the combined results from the 3 studies should be convincing. 2147 patients were included in this meta-analysis. The overall mortality was similar in the two groups (24.9%, 268/1075 in the laparoscopic group and 26.4%, 283/1072 in the open group) with no significance detected, as was the overall recurrence regardless of local or distant recurrence. Both the overall 5-year survival (about 74%) and 5-year disease-free survival (about 68%) were similar between the two groups, and no significant difference was demonstrated. From these results, laparoscopic colon cancer resection was demonstrated to be as safe and efficacious as the open surgery, as we expected.
In conclusion, compared to open surgery, laparoscopically assisted colectomy has been demonstrated to have short term advantages that include less pain, better pulmonary function, shorter time for return of bowel function (duration of postoperative ileus), less fatigue, improved convalescence, and more importantly reduced surgical morbidity and shorter duration of hospital stay. From the 3-year long-term data, laparoscopic surgery was also demonstrated to be as safe and efficacious as the conventional open approach. Our present work again demonstrated that, in terms of long-term outcomes of trials a the median follow-up more than 5 years, laparoscopic surgery is also as safe and efficacious as the conventional open approach. In addition, laparoscopic resection is associated with a modest additional cost, compared with open surgery. So regardless of the short-term outcomes or the long-term outcomes or even the cost-effectiveness, we could conclude that laparoscopic surgery is not inferior to the conventional open approach. From these analyses above, we think that for colon adenocarcinoma, laparoscopic assisted colectomy should be the preferred choice as appropriate.
Short-term advantages of laparoscopic colorectal surgery compared to conventional surgery are well known, however, it was uncertain whether there would be a long-term survival difference. Several large trials has been reported which report on long-term survival differences.
The objective of this systematic review is to assess that in the long term, laparoscopic-assisted colon resection for cancer is not inferior to open colectomy with respect to cancer survival and recurrence.
This meta-analysis suggests that laparoscopic surgery was as efficacious and safe as open surgery for colon cancer, based on the five-year data of the included randomized clinical trials.
For colon adenocarcinoma, laparoscopic assisted colectomy should be the preferred choice as appropriate.
The study was well structured and gives interesting information about the present status of laparoscopy and colon cancer. The main strength is the longer follow up of patients and the criteria to be included. I think this manuscript should be interesting for surgeons dealing with this disease.
Peer reviewers: Kevin Cheng-Wen Hsiao, MD, Assistant Professor, Colon and rectal surgery, Tri-Service General Hospital, No. 325, Sec. 2, Cheng-Kung Rd, Nei-Hu District, Taipei 114, Taiwan, China; De Aretxabala Xabier, Professor of Surgery, Universidad de Chile, Santos Dumont 999, Santiago, 8380000, Chile
S- Editor Tian L L- Editor O'Neill M E- Editor Lin YP
| 1. | Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43-66. [Cited in This Article: ] |
| 2. | Barkun JS, Barkun AN, Sampalis JS, Fried G, Taylor B, Wexler MJ, Goresky CA, Meakins JL. Randomised controlled trial of laparoscopic versus mini cholecystectomy. The McGill Gallstone Treatment Group. Lancet. 1992;340:1116-1119. [Cited in This Article: ] |
| 3. | Cooperman AM, Katz V, Zimmon D, Botero G. Laparoscopic colon resection: a case report. J Laparoendosc Surg. 1991;1:221-224. [Cited in This Article: ] |
| 4. | Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1:144-150. [Cited in This Article: ] |
| 5. | Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224-2229. [Cited in This Article: ] |
| 6. | Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA. 2002;287:321-328. [Cited in This Article: ] |
| 7. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [Cited in This Article: ] |
| 8. | Schwenk W, Böhm B, Müller JM. Postoperative pain and fatigue after laparoscopic or conventional colorectal resections. A prospective randomized trial. Surg Endosc. 1998;12:1131-1136. [Cited in This Article: ] |
| 9. | Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896-1900. [Cited in This Article: ] |
| 10. | Nelson H, Weeks JC, Wieand HS. Proposed phase III trial comparing laparoscopic-assisted colectomy versus open colectomy for colon cancer. J Natl Cancer Inst Monogr. 1995;51-56. [Cited in This Article: ] |
| 11. | Stage JG, Schulze S, Møller P, Overgaard H, Andersen M, Rebsdorf-Pedersen VB, Nielsen HJ. Prospective randomized study of laparoscopic versus open colonic resection for adenocarcinoma. Br J Surg. 1997;84:391-396. [Cited in This Article: ] |
| 12. | Milsom JW, Böhm B, Hammerhofer KA, Fazio V, Steiger E, Elson P. A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg. 1998;187:46-54; discussion 54-55. [Cited in This Article: ] |
| 13. | Curet MJ, Putrakul K, Pitcher DE, Josloff RK, Zucker KA. Laparoscopically assisted colon resection for colon carcinoma: perioperative results and long-term outcome. Surg Endosc. 2000;14:1062-1066. [Cited in This Article: ] |
| 14. | Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44-52. [Cited in This Article: ] |
| 15. | Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, Pique JM. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg. 2008;248:1-7. [Cited in This Article: ] |
| 16. | Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Nelson H. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655-662; discussion 662-664. [Cited in This Article: ] |
| 17. | A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [Cited in This Article: ] |
| 18. | Schwenk W, Haase O, Neudecker J, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;CD003145. [Cited in This Article: ] |
| 19. | Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, Guillou PJ, Thorpe H, Brown J, Delgado S. Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg. 2007;142:298-303. [Cited in This Article: ] |
| 20. | Kahnamoui K, Cadeddu M, Farrokhyar F, Anvari M. Laparoscopic surgery for colon cancer: a systematic review. Can J Surg. 2007;50:48-57. [Cited in This Article: ] |
| 21. | Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J. Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev. 2008;34:498-504. [Cited in This Article: ] |